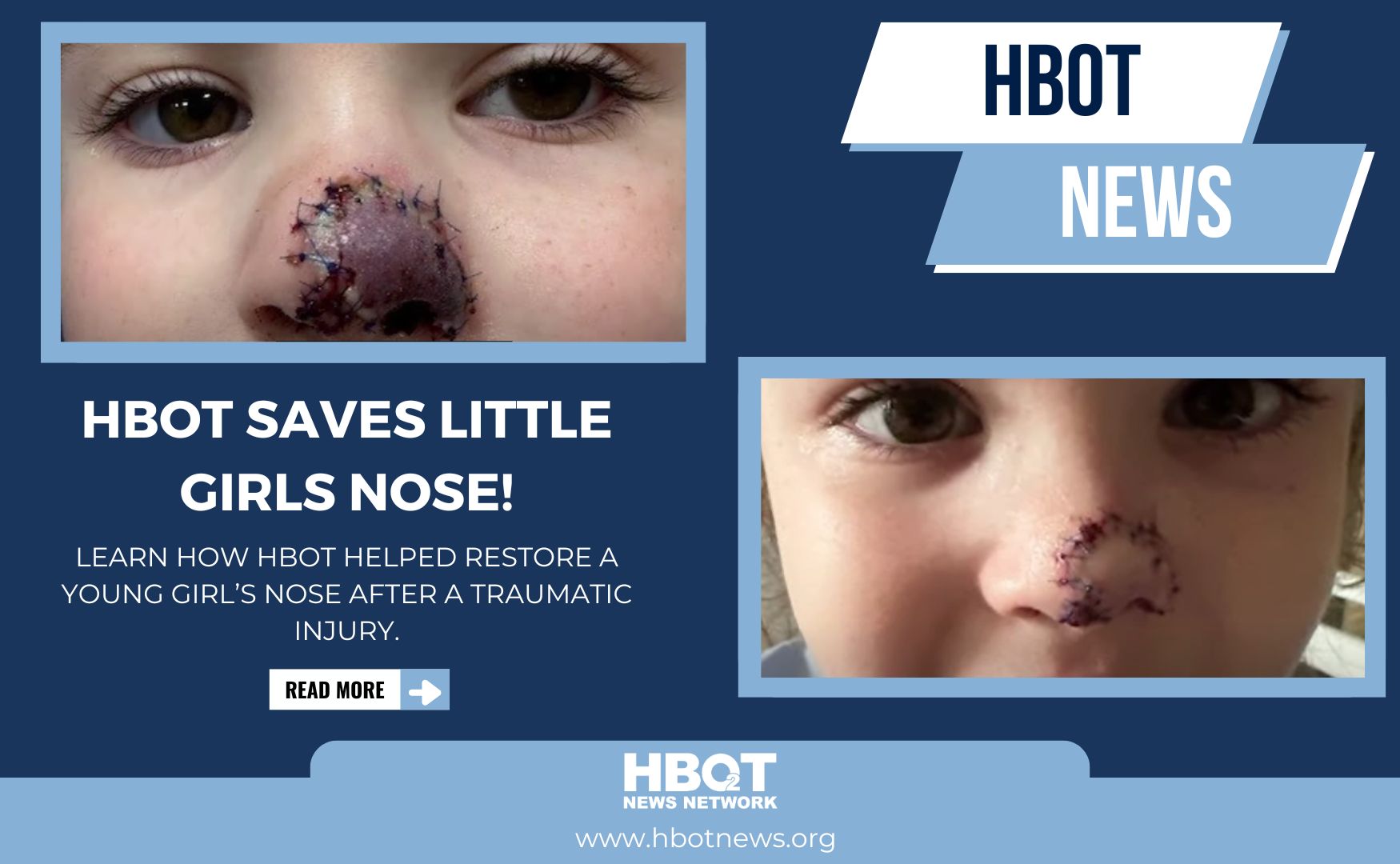
In a remarkable medical intervention, WWL-TV reports that Hyperbaric Oxygen Therapy (HBOT) was instrumental in saving a young girl’s nose following a severe dog bite. Five-year-old Lucy Nadler suffered a traumatic injury when a Labrador retriever bit off part of her nose. Surgeons reattached the severed portion, but the graft showed signs of necrosis due to inadequate blood flow. Facing limited options, Lucy’s mother, Dr. Jen Erbil, a rheumatologist, sought alternative treatments and turned to HBOT. Under the care of Dr. Paul Harch at Harch Hyperbarics in Metairie, Louisiana, Lucy underwent daily HBOT sessions. Remarkably, within 20 minutes of the initial treatment, the grafted tissue exhibited signs of revitalization, indicating restored blood flow. Over the course of a month, Lucy’s condition improved significantly, highlighting the potential of HBOT in complex reconstructive cases.
Understanding Hyperbaric Oxygen Therapy (HBOT)
HBOT involves administering 100% oxygen to patients within a pressurized chamber, typically at pressures between 1.5 to 3 times that of normal atmospheric pressure. This process significantly increases the amount of oxygen dissolved in the blood plasma, enhancing oxygen delivery to tissues. The elevated oxygen levels facilitate various physiological benefits, including reduced inflammation, accelerated wound healing, and the promotion of angiogenesis—the formation of new blood vessels.
Mechanisms of HBOT in Tissue Healing
- Enhanced Oxygen Delivery: Under normal conditions, oxygen is primarily transported by hemoglobin in red blood cells. HBOT increases the amount of oxygen dissolved in plasma, allowing it to diffuse more effectively into tissues, even those with compromised blood flow. This heightened oxygen availability supports cellular metabolism and accelerates healing processes.
- Reduction of Inflammation: HBOT has been shown to modulate inflammatory responses by decreasing the activity of pro-inflammatory cytokines and reducing neutrophil adhesion. This leads to diminished tissue swelling and inflammation, creating a more favorable environment for healing.
- Promotion of Angiogenesis: The therapy stimulates the release of growth factors and stem cells, which contribute to the formation of new blood vessels. This angiogenic effect enhances blood supply to injured tissues, supporting sustained healing and tissue regeneration.
- Antimicrobial Effects: Elevated oxygen levels can inhibit the growth of anaerobic bacteria and enhance the effectiveness of certain antibiotics, thereby reducing the risk of infection in healing tissues.



Application in Lucy’s Case
In Lucy’s situation, the reattached nasal tissue lacked sufficient blood flow, leading to tissue ischemia and necrosis. HBOT was employed to counteract these challenges by increasing oxygen delivery directly to the compromised tissue. The therapy’s ability to promote angiogenesis likely facilitated the development of new blood vessels, restoring perfusion to the grafted area. Additionally, the anti-inflammatory properties of HBOT would have reduced local swelling, further supporting tissue viability. The rapid improvement observed in Lucy’s condition underscores the potential of HBOT as a valuable adjunctive treatment in complex reconstructive surgeries and severe traumatic injuries.
Conclusion
Lucy Nadler’s recovery exemplifies the therapeutic potential of Hyperbaric Oxygen Therapy in enhancing tissue healing and viability following severe injuries. The scientific mechanisms underlying HBOT—including enhanced oxygen delivery, reduction of inflammation, promotion of angiogenesis, and antimicrobial effects—collectively contribute to its efficacy in such cases. As awareness and understanding of HBOT continue to grow within the medical community, its application may become more widespread, offering hope in situations where traditional treatments are limited.
Read More
Treat the Concussion: How HBOT Is Changing the Playbook for Concussions — An Interview with Dr. Daphne Denham
By HBOT News | Interview by Dr. Xavier FigueroaThe Big Idea For decades, concussion care has leaned on “rest and wait.” Dr. Daphne Denham believes that’s the wrong playbook. Drawing on years in trauma surgery and hyperbaric medicine, she argues that a concussion...
Understanding Hyperbaric Chambers: Types, Risks, and Safety Tips for Patients
Hyperbaric Oxygen Therapy (HBOT) is gaining recognition for its ability to support healing, reduce inflammation, and improve neurological and physical outcomes. While the science behind HBOT is compelling, patient safety is equally important. A critical aspect of...

Overcoming the Placebo Challenge: New Trial Confirms HBOT Benefits for TBI and PTSD
The Placebo Problem in HBOT Research Hyperbaric oxygen therapy (HBOT) has long shown promise in treating a range of neurological conditions, from traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) to post-COVID symptoms. Yet, clinical research on...

