News & Research
Hyperbaric Oxygen Therapy has been used for the better part of two centuries. Search our arhives below for past HBOT news and research or scroll down for the latest.
The Latest HBOT News & Research
Increasing Veteran’s Access to Hyperbaric Oxygen Treatments
The new MISSION Act, passed by Congress last year, could pave the way for Hyperbaric Oxygen Therapy (HBOT) to be covered by the VA. In general, the act is making better healthcare more easily accessible to veterans. There are a couple of specific...
Treatment of Traumatic Brain Injury With Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) is defined as the use of oxygen at higher than atmospheric pressure for the treatment of underlying disease processes and the diseases they produce. Modern HBOT in which 100% O2 is breathed in a pressurized chamber dates back to the 1930s, when it was first used for treatment of decompression illness in divers. There are currently 13 FDA-approved uses for HBOT, including decompression illness, gas gangrene, air embolism, osteomyelitis, radiation necrosis, and the most recent addition—diabetic ulcers. HBOT can dramatically and permanently improve symptoms of chronic TBI months or even many years after the original head injury. This assertion is generally met with skepticism within the medical establishment because we have been taught for generations that any post-concussion symptoms persisting more than 6 months or so after a head injury are due to permanent brain damage that cannot be repaired.
Clinical Trial – Comparison of Clorotekal and Bupivacaine for Short Obstetric Surgery
The following obstetric procedures are commonly performed with spinal anesthesia on labor and
delivery: bilateral tubal ligation, external cephalic version, cerclage insertion, cerclage
removal, minimally invasive fetal surgery, and evacuation of retained products of conception.
Bupivacaine is currently the standard spinal medication for these procedures because of its
long history of safe use, its low incidence of transient neurologic symptoms, and its ability
to provide a dependable, dense block with a high degree of maternal satisfaction. While
bupivacaine has the aforementioned advantages, it unfortunately has a long duration of
action, up to 240-380 minutes, which far exceeds the time necessary to complete most
obstetric procedures. Clorotekal®, the first Food and Drug Administration approved
chloroprocaine solution created for spinal injection, is a potential alternative. When
compared with bupivacaine spinals, chloroprocaine spinals have been shown to facilitate
clinically significant shorter times to resolution of motor and sensory block, first
ambulation, micturition, and discharge readiness. The objective of this study is to determine
if a strategy of spinal anesthesia with chloroprocaine will reduce the duration of motor
block, compared with equivalent block with hyperbaric bupivacaine..
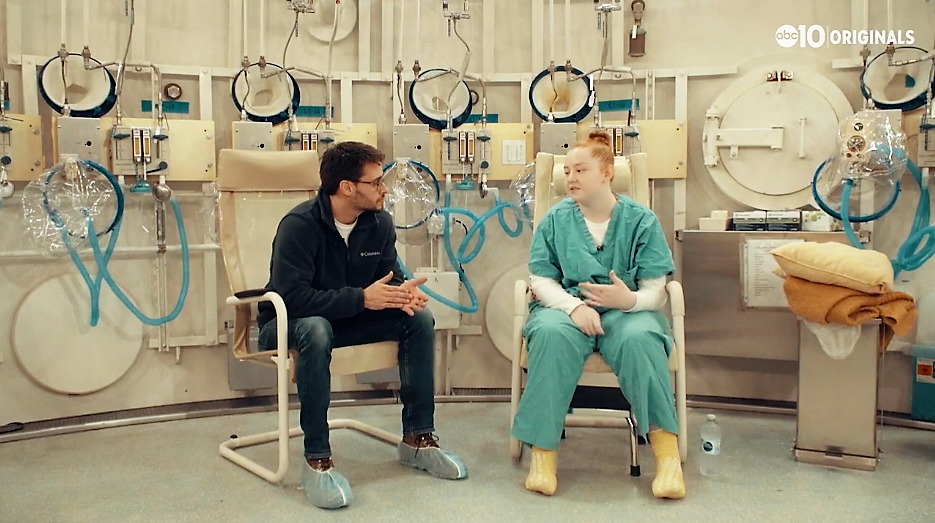
Healing under pressure: Inside a military hyperbaric chamber
At 16, she had a stroke. At 17, her town burned in the Camp Fire. Now, as her community rebuilds, she's healing thanks to hyperbaric therapy. SACRAMENTO, Calif — February 2, 2017, started off as an ordinary day for the Pipkin Family. Patrick and...
Clinical Trial – High-flow Oxygen for Vaso-occlusive Pain Crisis
Sickle cell disease (SCD) is characterized by recurrent vaso-occlusive pain crisis (VOC),
which may evolve to acute chest syndrome (ACS), the most common cause of death among adult
patients with SCD. Currently, there is no safe and effective treatment to abort VOC or
prevent secondary ACS. Management of VOC mostly involve a symptomatic approach including
hydration, analgesics, transfusion, and incentive spirometry, which was investigated in a
very limited number of patients (<30).
The polymerisation of HbS is one major feature in the pathogenesis of vaso-occlusion. Among
factors determining the rate and extent of HbS polymer formation, the hypoxic stimulus is one
of the most potent and readily alterable. Current guidelines recommend oxygen therapy in
patients with VOC in order to maintain a target oxygen saturation of 95%. Low-flow nasal
oxygen (LFNO) is routinely used to achieve this normoxia approach, particularly in patients
at risk of secondary ACS because they may experience acute desaturation. In contrast, various
case series suggest a potential beneficial role of intensified oxygen therapy targeting
hyperoxia for the management of VOC, particularly with the use of hyperbaric oxygen, but the
latter is difficult to implement in routine clinical practice.
A recent high-flow nasal oxygen (HFNO) technology allows the delivery of humidified gas at
high fraction of inspired oxygen (FiO2) through nasal cannula. The FiO2 can be adjusted up to
100% (allowing hyperoxia that may reverse sickling) and the flow can be increased up to 60
L/min (which generates positive airway pressure and dead space flushing, that may prevent
evolution of VOC towards ACS by alleviating atelectasis and opioid-induced hypercapnia). In
patients with acute respiratory failure, HFNO has been shown to improve patient's comfort,
oxygenation, and survival as compared to standard oxygen or non-invasive ventilation.
The aim of the present study is to test the efficacy and safety of HFNO for the management of
VOC and prevention of secondary ACS. The investigators will use a multi-arm multi-stage
(MAMS) design to achieve these goals. HFNO will be delivered through AIRVO 2 (Fisher and
Paykel Healthcare, New Zealand), a device that incorporates a turbine allowing its use in
hospital wards.
Clinical Trial – Hyperbaric Oxygen Therapy and Allogeneic Peripheral Blood Stem Cell (PBSC) Transplant
Subjects with Acute Myeloblastic Leukemia (AML) and myelodysplastic syndrome (MDS) who are
considered eligible for allogeneic stem cell transplant by the transplant team at WCI (Wilmot
Cancer Institute)will be enrolled in the study. Patients will receive Melphalan on day -2 and
HBO (Hyperbaric Oxygen) therapy on day 0 of the transplant. After neutrophil recovery is
documented, the patients will be seen in clinic at least weekly through day +100.
Clinical Trial – Effect of Hyperbaric Oxygen Therapy on Microcirculation
Previous studies shoes that hyperoxia alters microcirculation.The investigators hypothesize
that hyperbaric may restore microcirculation integrity. This hypothesis is supported by a
recent study in rabbits, but no data exists for humans.
The study will expose fifteen healthy volunteers to a succession of different fraction of
inspired oxygen and barometric pressure and assess microcirculatory and macrocirculatory
changes via sidestream dark field videomicroscopy, near-infrared spectroscopy, Laser Doppler,
transthoracic echocardiography and bio-impedancemetry at every step.
Clinical Trial – 3 Local Anesthetics for Spinal Anesthesia in Primary Total Hip Arthroplasty
Spinal anesthesia is commonly utilized for hip replacement surgery. Different medications
used for spinal anesthesia work for different lengths of time. This study will compare three
different spinal anesthesia medications in patients having hip replacement surgery to see if
patients are able to get out of bed and walk earlier after surgery with one medication versus
the others.
Clinical Trial – Comparision of Different Doses of Dexmedetomidine With Low Dose Bupivacaine in Selective Spinal Anesthesia.
The charactereistics of a spinal block varies with the dose of local anaesthetic and the
adjuvant used. Literature review did not show comparison of different doses of
dexmedetomidine with low-dose bupivacaine in saddle block. The rationale of this study is to
determine an optimum dose of dexmedetomidine which in combination with low dose bupivacaine
would provide satisfactory block with hemodynamic stability. This would be beneficial for
patients scheduled for turp, as these pts are mostly elderly with various comorbidities.