HBOT Conversations:
Dr. Paul Harch & 8,101 Genes
He is the author of The Oxygen Revolution and is considered an International expert and pioneer in the field of Hyperbaric Oxygen Therapy (HBOT). His informative, and comprehensive guide on HBOT has helped countless souls better understand what HBOT is and how it directly affects the body at the genetic level.
This episode on 8,101 genes is the eighth in a nine episode series that will be released weekly with Dr. Harch.
Watch the Podcast
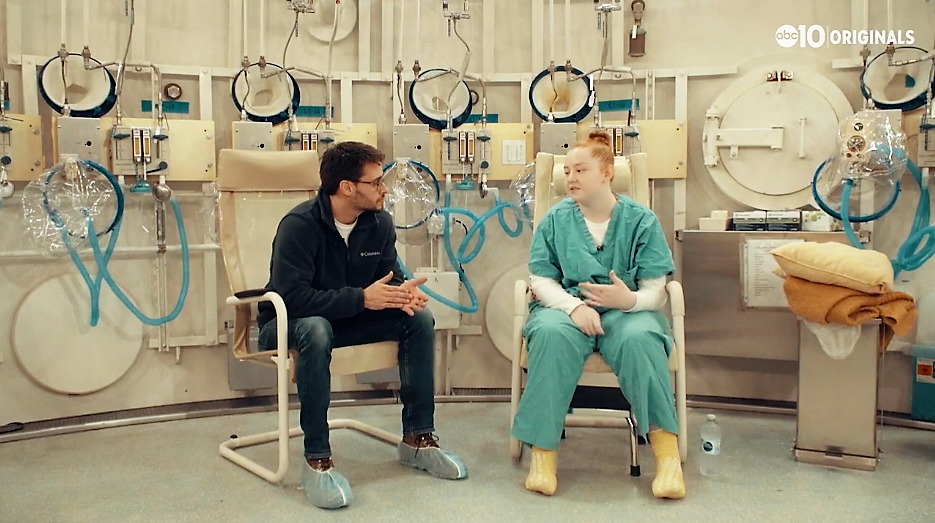
In episode 8 of 9, host Edward di Girolamo speaks with world renowned HBOT expert, Dr. Paul G. Harch, about aging and the 8,101 genes HBOT affects.
di Girolamo starts this conversation with Dr. Harch bringing up the 8,101 genes that are activated by Hyperbaric Oxygen Therapy. The discussion leads to talk of Big Pharma, telomeres, reparative gene process, patents, and successful business models for HBOT clinics.
Dr. Harch explains that Hyperbaric Oxygen Therapy affects 8,101 of our genes, and it’s doing so on a different level for the ones that are overactive and abnormal in the disease process. He speaks of a 2004 lecture he gave to A4M about the effects of HBOT on longevity; and asks, “Where is senescence and aging based?”, answering with, “It’s in our DNA”. Dr. Harch dives in to how HBOT turns on our genes to grow new tissue and stimulates cellular repair and regeneration. di Girolamo agrees and brings up a different past lecture from Dr. Harch where Harch referred to Hyperbaric Oxygen Therapy as the ‘Fountain of Youth‘.
This series ends with Dr. Harch discussing a Buffalo VA study, and how the study subjects (comprised of older veterans) literally came alive and started propositioning nurses after Hyperbaric Oxygen Therapy treatments. He explained this is why no follow-up study was ever done because they weren’t expecting such and didn’t know what to do. Makes sense…. studies have shown success in HBOT treating erectile dysfunction.
If you are searching for the Fountain of Youth and ready to activate 8,101 genes in your body —- find a Hyperbaric Oxygen Therapy clinic near you.
Subscribe Now, It’s Free!
Guest
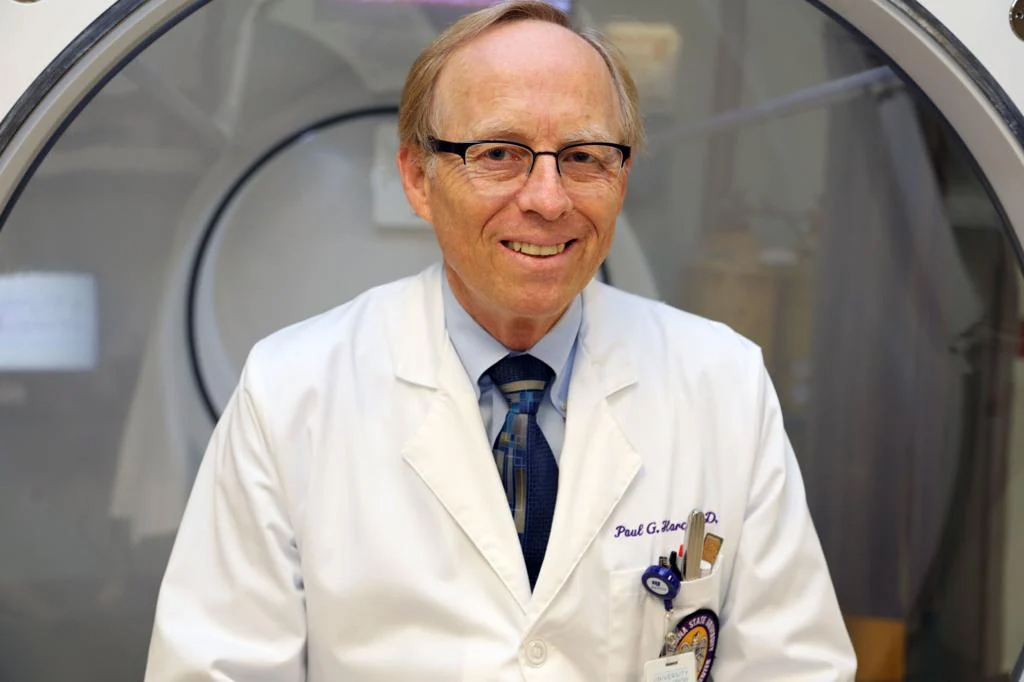
Dr. Paul G. Harch, MD
Dr. Harch initiated and continues to be a private practice that has resulted in the largest case experience in neurological hyperbaric medicine in the world. In this practice, he adapted the concepts of conventional hyperbaric oxygen therapy to wounds in the central nervous system, which spawned the subsequent academic and research practice. Harch HBOT is the best place to receive oxygen therapy treatments, and patients have traveled from more than 50 countries to be treated by Dr. Harch himself.
Harch HBOT – Hyperbaric Oxygen Therapy Clinic
5216 Lapalco Blvd.
Marrero, LA
504-309-4948
hbot@hbot.com
https://hbot.com/
Recent HBOT News
Healing under pressure: Inside a military hyperbaric chamber
At 16, she had a stroke. At 17, her town burned in the Camp Fire. Now, as her community rebuilds, she's healing thanks to hyperbaric therapy. SACRAMENTO, Calif — February 2, 2017, started off as an ordinary day for the Pipkin Family. Patrick and Stacey Pipkin just...
Clinical Trial – High-flow Oxygen for Vaso-occlusive Pain Crisis
Sickle cell disease (SCD) is characterized by recurrent vaso-occlusive pain crisis (VOC),
which may evolve to acute chest syndrome (ACS), the most common cause of death among adult
patients with SCD. Currently, there is no safe and effective treatment to abort VOC or
prevent secondary ACS. Management of VOC mostly involve a symptomatic approach including
hydration, analgesics, transfusion, and incentive spirometry, which was investigated in a
very limited number of patients (<30).
The polymerisation of HbS is one major feature in the pathogenesis of vaso-occlusion. Among
factors determining the rate and extent of HbS polymer formation, the hypoxic stimulus is one
of the most potent and readily alterable. Current guidelines recommend oxygen therapy in
patients with VOC in order to maintain a target oxygen saturation of 95%. Low-flow nasal
oxygen (LFNO) is routinely used to achieve this normoxia approach, particularly in patients
at risk of secondary ACS because they may experience acute desaturation. In contrast, various
case series suggest a potential beneficial role of intensified oxygen therapy targeting
hyperoxia for the management of VOC, particularly with the use of hyperbaric oxygen, but the
latter is difficult to implement in routine clinical practice.
A recent high-flow nasal oxygen (HFNO) technology allows the delivery of humidified gas at
high fraction of inspired oxygen (FiO2) through nasal cannula. The FiO2 can be adjusted up to
100% (allowing hyperoxia that may reverse sickling) and the flow can be increased up to 60
L/min (which generates positive airway pressure and dead space flushing, that may prevent
evolution of VOC towards ACS by alleviating atelectasis and opioid-induced hypercapnia). In
patients with acute respiratory failure, HFNO has been shown to improve patient's comfort,
oxygenation, and survival as compared to standard oxygen or non-invasive ventilation.
The aim of the present study is to test the efficacy and safety of HFNO for the management of
VOC and prevention of secondary ACS. The investigators will use a multi-arm multi-stage
(MAMS) design to achieve these goals. HFNO will be delivered through AIRVO 2 (Fisher and
Paykel Healthcare, New Zealand), a device that incorporates a turbine allowing its use in
hospital wards.
Clinical Trial – Hyperbaric Oxygen Therapy and Allogeneic Peripheral Blood Stem Cell (PBSC) Transplant
Subjects with Acute Myeloblastic Leukemia (AML) and myelodysplastic syndrome (MDS) who are
considered eligible for allogeneic stem cell transplant by the transplant team at WCI (Wilmot
Cancer Institute)will be enrolled in the study. Patients will receive Melphalan on day -2 and
HBO (Hyperbaric Oxygen) therapy on day 0 of the transplant. After neutrophil recovery is
documented, the patients will be seen in clinic at least weekly through day +100.