HBOT Conversations:
Dr. Paul Harch & Strokes
Dr. Paul G. Harch, M.D. has used hyperbaric oxygen therapy to treat more than 100 different conditions, including stroke, dementia, autism, and traumatic brain injury. His goal is to help his patients get their lives back using hyperbaric oxygen therapy.
He is the author of The Oxygen Revolution and is considered an International expert and pioneer in the field of Hyperbaric Oxygen Therapy (HBOT). His informative, and comprehensive guide on HBOT has helped countless souls better understand what HBOT is and how it directly affects the body at the genetic level.
This episode on strokes is the sixth in a nine episode series that will be released weekly with Dr. Harch.
Watch the Podcast
In episode 6 of 9, host Edward di Girolamo speaks with world renowned HBOT expert, Dr. Paul G. Harch about strokes. Dr. Harch explains that Hyperbaric Oxygen Therapy is hands-down the most effective therapy to treat the debilitating after-effects of a stroke.
But what exactly happens during a stroke and how can HBOT help?
We have more blood flow happening in the parts of the brain that are working hard to coordinate the movement of muscles, the formation of words, etc. Dr. Harch refers to this blood flow like the RPMs in a motor, the blood flow revs up and increases as we increase our movement & activity. However, having a stroke causes a blockage or lowering of blood flow to the brain, which can cause “electrical silence” – when the cells get to a point at about 60% reduction in blood flow where they no longer have enough oxygen (and blood flow, sugar, and fat) to generate electrical signals. These cells do not die, they live in a state of idling.
Dr. Harch explains there was a strong misunderstanding among the medical community that brain cells were either alive or dead after a stroke or injury. Over the years, HBOT has proven to the medical community that brain cells can just be in an idle/injured state and under the right conditions (like oxygen + pressure) they can be revived to function again.
Dr. Harch speaks in detail of two HBOT success stories of stroke patients getting significantly better even 10 years+ post-stroke —-
- A 60 year old woman who was 14 years post-stroke; paralyzed, drooling, can’t eat, no speech, totally dependent, and spending her days in a Geri Chair. Over the next 16 months they treated her periodically with Hyperbaric Oxygen Therapy and continue to do blood flow brain scans on her before and after the treatments. The deadest area of her brain immediately started to light up with blood flow after just the first treatment. She eventually reacquired her speech, stop drooling, and they were able to get her up moving with assisted ambulation.
- It was early 1990s and a Gentlemen called, Mr. H, who was 12 years post-stroke came into Dr. Harch’s clinic; completely mute with no ability to talk or communicate, unable to move at all; he just laid in bed all day. Eventually his wife had to put him in a nursing home, where he was referred to Hyperbaric Oxygen Therapy for the horrendous bed sore wounds he had developed. They started treatment with HBOT and continued to treat him, even after the bed sores started healing. The medical staff noticed that after about 18 HBOT treatment sessions he was now waving to the doctors and nurses as he was being wheeled through the doors on a stretcher. So they keep treating him with HBOT…… 10 more treatments and he starts talking. By flooding his body with oxygen under the pressure conditions of hyperbarics, for the first time in 12 years his brain started to wake up.
Moving away from topic of stroke, but still focusing on the power of Hyperbarics and success stories, di Girolamo tells Dr. Harch that he once said to Bill Duncan, “From what I understand of Hyperbaric Oxygen, the only thing it can’t do is bring back the dead.” And Bill responded with, “that’s not entirely true”. This opened the door for Dr. Harch to talk about a bizarre and fascinating Hyperbaric Oxygen Therapy success story from the 1980s. A diver was about 80 – 90 feet down in the Mississippi River with an airlift, as part of a mission to salvage a new tugboat that sunk. As the dive team was suctioning silt to loosen it up from the sunken boat, this diver’s helmet came off when he got sucked up against the bar of the dredging device. It took a long time for other divers to find him, and when they do bring him up he’s “dead as dead can be”. Without really knowing exactly why he’s in cardiac arrest, they immediately put him in a hyperbaric chamber in hopes that it would help stabilize him from any decompression sickness. They put an oxygen mask on him and take him to six atmospheres of pressure (clinical chambers go to maximum 3) – that’s 165 feet of pressure! He sparked up and came to life! He had been in cardiac arrest for 25 minutes. He went on to live a healthy life with a bright IQ. Later studies have involved guinea pigs, rats, and swine – some as much as 25 minutes after cardiac arrest and success with resuscitation after Hyperbaric Oxygen Therapy. So, yes there’s scientific proof that HBOT can even bring back the dead.
Dr. Harch stresses at the end of this HBOT Conversation that it’s never too late to get HBOT. Obviously, the sooner the better; but it still works on patients many many years post-stroke. There are approximately 800,000 strokes per year in the United States — it’s a huge number. And unfortunately only an extremely small amount of stroke victims receive Hyperbaric Oxygen Therapy. Dr. Harch classifies HBOT as “hope for the hopeless”.
If you or a loved one has recently experienced a stroke, we encourage you to better understand how Hyperbaric Oxygen Therapy can help wake up a post-stroke brain. We wish you the best as you find hope in HBOT.
Subscribe Now, It’s Free!
Guest
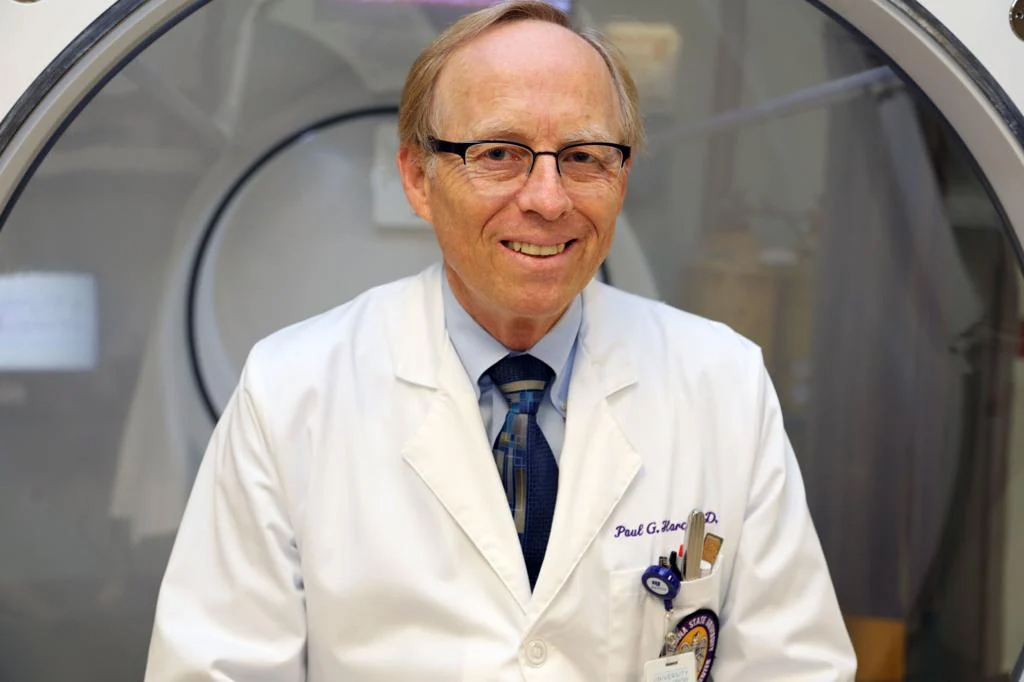
Dr. Paul G. Harch, MD
Dr. Harch initiated and continues to be a private practice that has resulted in the largest case experience in neurological hyperbaric medicine in the world. In this practice, he adapted the concepts of conventional hyperbaric oxygen therapy to wounds in the central nervous system, which spawned the subsequent academic and research practice. Harch HBOT is the best place to receive oxygen therapy treatments, and patients have traveled from more than 50 countries to be treated by Dr. Harch himself.
Harch HBOT – Hyperbaric Oxygen Therapy Clinic
5216 Lapalco Blvd.
Marrero, LA
504-309-4948
hbot@hbot.com
https://hbot.com/
Recent HBOT News
Senate VA Committee Passes Legislation on Hyperbaric Oxygen Therapy
Back in October 2019, at Senator Cramer’s invitation, VA Secretary Robert Wilkie and the Senator toured Healing with Hyperbarics of North Dakota, a Fargo-based HBOT clinic. Cramer states, “The primary point of the federal government is the defense of our nation. Part...
Clinical Trial – the Use of Magnesium Sulfate for Prevention of Postspinal Shivering
Shivering is an unpleasant experience after spinal anesthesia. Shivering is defined as an
involuntary, repetitive activity of skeletal muscles. The mechanisms of shivering in patients
undergoing surgery are mainly intraoperative heat loss, increased sympathetic tone, pain, and
systemic release of pyrogens. Spinal anesthesia significantly impairs the thermoregulation
system by inhibiting tonic vasoconstriction, which plays a significant role in temperature
regulation. Spinal anesthesia also causes redistribution of core heat from the trunk (below
the block level) to the peripheral tissues. These two effects predispose patients to
hypothermia and shivering. The median incidence of shivering related to regional anesthesia
observed in a review of 21 studies is 55%. Shivering increases oxygen consumption, lactic
acidosis, carbon dioxide production, and metabolic rate by up to 400%. Therefore, shivering
may cause problems in patients with low cardiac and pulmonary reserves. The best way to avoid
these intraoperative and postoperative shivering-induced increases in hemodynamic and
metabolic demands is to prevent shivering in the first place. Although magnesium is among
several pharmacological agents used for the treatment of shivering, its effects on prevention
of shivering during central neuraxial blockade have not been evaluated to date. Henceforth,
the aim of this study was to evaluate the effect of magnesiume on shivering during spinal
anesthesia.
Aim:
to compare the efficacy of intravenous versus intrathecal magnesium sulphate for prevention
of post spinal shivering in adult patients undergoing elective lower limb orthopedic
surgeries.
Clinical Trial – Comparing the Effects of Levobupivacaine and Bupivacaine in Saddle Spinal Anesthesia
İn this study; it was aimed to investigate the effects of equipotent doses of hyperbaric
bupivacaine and hyperbaric levobupivacaine in outpatient anorectal surgery under saddle
block. Sixty patients between the age of 18- 50 and in the risk group of ASA I-II included in
the study. 7,5 mg of 0,5% hyperbaric bupivacaine or 7,5 mg of 0,5% hyperbaric levobupivacaine
injected into the intrathecal space in sitting position through L4-L5 or L5-S1 intervertebral
space in 30 seconds. All patients kept in sitting position for 5 minutes with aid after
intrathecal injection and than layed in supine position, finally they positioned in prone
jack-knife. Hemodynamic parameters like NIBP, HR, SpO2, sensory and motor block
characteristics, duration of analgesia, time of first voiding, mobilization time, patient and
surgeon satisfaction, adverse effects and discharge time were recorded during and after
surgery.

