
Hyperbaric Oxygen Therapy (HBOT) is gaining recognition for its ability to support healing, reduce inflammation, and improve neurological and physical outcomes. While the science behind HBOT is compelling, patient safety is equally important. A critical aspect of safety lies in understanding the different types of hyperbaric chambers, how they operate, their risks, and how patients can ensure they are receiving care from qualified providers.
Types of Hyperbaric Chambers
HBOT chambers are broadly categorized by capacity (monoplace vs. multiplace) and construction (hard-shell vs. soft-shell). Hard-shell chambers are typically medical-grade and used in clinical settings, while soft-shell ones are often for milder, non-medical applications. Beyond these, there are specialized chambers for diving medicine and emergency use.
Monoplace Chambers
Hard-Shell (Medical-Grade)
Rigid acrylic or plexiglass tubes designed for one patient lying down. They are FDA-approved for 14 recognized conditions and can reach up to ~3.0 ATA. The entire chamber is pressurized with 100% oxygen, delivering strong therapeutic effects but creating a higher fire risk. Because these chambers are fully enclosed, patients may experience claustrophobia, though many facilities provide communication systems to ease anxiety. Despite the risks, hard-shell monoplace chambers remain the most widely used type of HBOT chamber in outpatient clinics due to their effectiveness and accessibility.

Soft-Shell (“Mild”)
Portable, inflatable chambers typically operating at 1.3–1.5 ATA, sometimes with an oxygen concentrator. These are not FDA-approved for most medical conditions (except acute mountain sickness). While more accessible, they cannot achieve therapeutic pressures needed for most HBOT indications. They are often marketed for wellness, athletic recovery, or anti-aging, but scientific evidence supporting these uses remains limited. Because they are frequently used outside of medical supervision, safety standards and effectiveness can vary widely.

Multiplace Chambers
Multiplace chambers are larger, room-sized units designed to treat multiple patients at once. The chamber itself is filled with compressed air, while each patient breathes 100% oxygen through a mask or hood. These chambers typically operate at 2.0–3.0 ATA and offer several advantages, including direct supervision by trained staff, reduced claustrophobia due to the open space, and the ability to provide “air breaks” to lower the risk of oxygen toxicity. Because multiple people are treated at the same time, safety protocols must be strictly enforced, especially fire prevention, and patients must wear their masks consistently to ensure effective therapy.

Recompression/Diving Chambers
Primarily used for decompression sickness and diving injuries, these chambers operate at higher pressures—typically up to 2.8 bar (about 2.8 ATA, equal to 18 meters of seawater depth). They resemble multiplace chambers in design but are built to withstand the greater pressures required for diving medicine. Treatments follow strict “treatment tables” that carefully control pressure and oxygen exposure to safely eliminate excess nitrogen from the body, and unlike standard HBOT sessions that last 45–120 minutes, recompression dives are much longer—often running 4 to 5 hours or more depending on symptoms.

Hyperbaric Stretchers
Portable and collapsible, hyperbaric stretchers are used in military, transport, or remote settings and can reach about 2.3 bar above ambient pressure (roughly 3.3 ATA) while being pressurized with air. Patients breathe oxygen through a demand mask, which provides short-term stabilization but not the continuous high-dose delivery of medical-grade chambers. Their range is limited because they are small, confined units designed for emergencies, not extended treatments, with minimal monitoring compared to clinical chambers. They are best for stabilizing and transporting patients until they reach a hard-shell monoplace or multiplace chamber, not as substitutes for a full HBOT protocol.

Pressurization Methods: Air vs. Oxygen
Hyperbaric chambers can be pressurized using either 100% oxygen or compressed air, and the choice of pressurization method plays a central role in both safety and therapeutic effectiveness. Treatments are measured in atmospheres absolute (ATA), where 1 ATA equals the normal air pressure at sea level (14.7 psi or 760 mmHg). When a chamber is pressurized above 1 ATA, more oxygen dissolves into the bloodstream and tissues, delivering a therapeutic dose that cannot be achieved by simply breathing oxygen at normal pressure. The Undersea and Hyperbaric Medical Society (UHMS) defines a true hyperbaric environment as any treatment delivered at 1.4 ATA or higher, since below this threshold the oxygen exposure is no greater than that provided by a non-rebreather mask at sea level.
To achieve pressures above 1.0 ATA, chambers are mechanically sealed and then gradually compressed with either pure oxygen or air, depending on the chamber design. This process increases the atmospheric pressure inside the chamber and directly determines the amount of oxygen available for absorption into the body.
Pressurization with Oxygen
In monoplace chambers, the entire chamber is filled with 100% oxygen. This method provides a direct and highly concentrated oxygen environment that significantly raises arterial oxygen levels. At sea level, breathing 100% oxygen increases arterial oxygen to about 760 mmHg, but under hyperbaric conditions these levels can exceed 1,500 mmHg. This delivers powerful therapeutic outcomes, making monoplace chambers effective for many FDA-approved conditions. However, the oxygen-enriched environment creates a much higher fire risk, requiring strict adherence to safety protocols and careful monitoring throughout treatment.
Pressurization with Air
Multiplace chambers operate differently. Instead of filling the entire space with oxygen, they are pressurized with compressed air, typically containing 19–23% oxygen, similar to normal atmospheric air. Patients then breathe 100% oxygen through hoods, masks, or breathing tubes, which allows multiple people to be treated safely at the same time. Because the chamber itself is not oxygen-enriched, the fire hazard is greatly reduced. However, this method depends on individualized oxygen delivery systems, and therapy effectiveness requires that patients wear their hoods or masks consistently and correctly.
Balancing Pressure and Safety
One of the most important aspects of HBOT is finding the right balance between enough pressure to achieve benefits and not so much pressure that it causes complications. The amount of oxygen your body absorbs during therapy depends directly on how much the chamber is pressurized. For example, at 1.5 ATA (about the pressure you’d experience 16 feet under water), oxygen levels in the blood rise well above normal. At 2.0 ATA (about 33 feet under water), the oxygen levels are even higher—nearly double what you would get at 1.5 ATA. This extra boost can make a big difference in how effectively the therapy supports healing, especially for wounds, infections, or neurological recovery.
But with higher pressure and higher oxygen comes increased risk. If the body is exposed to too much oxygen for too long, it can overstimulate the nervous system or irritate the lungs, leading to a condition known as oxygen toxicity. Symptoms may include dizziness, vision changes, coughing, or, in rare cases, seizures. This doesn’t mean higher pressures are unsafe—it simply means they must be used carefully.
To minimize risks, treatments are always delivered according to strict medical protocols. The pressure inside the chamber is increased and decreased slowly to protect the ears and lungs, and treatment times are carefully set based on the condition being treated. In multiplace chambers, patients may take short “air breaks,” breathing regular air for a few minutes during therapy to help the body process oxygen more safely. Continuous monitoring by trained staff ensures that if any discomfort arises—such as ear pain or shortness of breath—the session can be adjusted immediately.
In short, higher pressure equals more healing power, but also greater responsibility for safety. The goal of HBOT is to maximize therapeutic benefits while keeping every treatment well within safe limits.
Risks Across All Chambers
While each chamber type has specific concerns, there are general risks that apply to all forms of HBOT:
Barotrauma: One of the most common risks of HBOT, barotrauma occurs when pressure changes cause damage to the ears, sinuses, or, in rare cases, the lungs. Patients may feel ear fullness or sinus discomfort as pressure increases. Slow, controlled compression and decompression, combined with techniques like swallowing or yawning to equalize pressure, help prevent injury.
Oxygen Toxicity: Breathing very high concentrations of oxygen for extended periods can overstimulate the nervous system or irritate the lungs. In severe cases, this may lead to seizures, coughing, or chest discomfort. Fortunately, these events are rare, and careful monitoring of treatment time, oxygen dosage, and scheduled “air breaks” in multiplace chambers significantly reduce the risk.
Fire Hazards: Oxygen-rich environments greatly increase the potential for combustion. Even a small spark can ignite materials inside the chamber if safety protocols are ignored. To minimize this risk, all facilities strictly prohibit lighters, open flames, electronic devices, or any flammable substances inside or near the chamber. Medical-grade chambers are also built to meet NFPA (National Fire Protection Association) standards to further enhance safety.
Claustrophobia or Anxiety: Monoplace chambers are long, narrow acrylic cylinders designed for a single patient. While many find the experience relaxing, others may feel confined or anxious. This can manifest as restlessness, elevated heart rate, or even panic. Providers often mitigate this by offering communication systems, calming techniques, and, in multiplace chambers, a more open environment with staff present inside.
Improper Screening: Not everyone is a candidate for HBOT. Patients with untreated pneumothorax (collapsed lung), uncontrolled seizures, or certain lung conditions may face increased risk during treatment. Proper medical screening before beginning HBOT is critical to identify contraindications and ensure safety.
Monoplace vs. Multiplace: Comparing Safety and Efficacy
Safety
When it comes to hyperbaric chambers, safety depends on both the design of the chamber and how it is operated. Although Hyperbaric Oxygen Therapy (HBOT) is considered generally safe—with adverse events occurring in only about 0.4–2% of treatments—different chamber types carry different risks. Most side effects are mild, such as temporary ear pressure or sinus discomfort, but understanding the safety profiles of each chamber helps patients make informed choices.
Monoplace Chambers
Monoplace chambers are filled entirely with 100% oxygen, which makes them highly effective but also raises safety concerns. The oxygen-rich environment creates a greater fire hazard compared to other chambers. For this reason, strict rules prohibit electronics, flammable items, or anything that could spark inside the chamber. Patients may also experience claustrophobia because these chambers are enclosed, single-person cylinders. While risks are generally well managed in accredited facilities, higher oxygen exposure in monoplace chambers also slightly increases the chance of oxygen toxicity if sessions are not carefully monitored. Tragic accidents in hyperbaric chambers are extremely rare, but they have occurred. In 2025, a monoplace chamber in Michigan caught fire, leading to one fatality and serious injuries. Investigators determined this was not a freak accident but the result of serious safety breaches, including the use of flammable materials, lack of proper oversight, and failure to follow established protocols. While such incidents are exceptionally uncommon—thanks to rigorous safety standards set by organizations like the NFPA (National Fire Protection Association) and the Undersea and Hyperbaric Medical Society (UHMS)—this tragedy serves as a powerful reminder that hyperbaric therapy requires zero tolerance for lapses. Strict adherence to safety procedures, proper accreditation, and continuous medical supervision are non-negotiable to ensure patient safety.
Multiplace Chambers
Multiplace chambers are pressurized with air, and patients breathe oxygen through masks or hoods. This design significantly reduces the fire hazard because the chamber itself is not oxygen-rich. In addition, trained staff are often present inside the chamber, allowing patients to receive direct supervision. Safety protocols are easier to enforce in this environment, and the larger space helps patients who feel anxious or confined in monoplace chambers. However, because multiple people are treated at the same time, mask compliance is critical—removing the mask reduces therapy effectiveness.
Soft-Shell Chambers
Soft-sided or “mild” chambers are typically pressurized with air at lower levels (around 1.3–1.5 ATA). Because of the lower pressure, the risk of oxygen toxicity or barotrauma is minimal. On the surface, this makes them seem safer; however, these chambers usually lack medical oversight, and they are not FDA-approved for most conditions. While they are often marketed for home or wellness use, they do not deliver therapeutic oxygen levels recognized as true HBOT. This means that, although lower in risk, they are not effective substitutes for medical-grade chambers and should never be used without proper safety precautions.
Efficacy
While safety determines whether treatment is delivered responsibly, efficacy determines whether it works as intended. Here, chamber type again makes a major difference. The level of pressure a chamber can achieve, combined with how oxygen is delivered, directly impacts how much oxygen reaches the body’s tissues. In other words, not all chambers provide the same therapeutic dose, which is why medical-grade chambers stand apart from soft-shell or non-approved systems.
Monoplace Chambers
Because the entire chamber is filled with 100% oxygen at pressures between 2.0 and 3.0 ATA, monoplace chambers deliver strong therapeutic results. They are effective for all 14 UHMS-approved conditions, including chronic wound healing, radiation injury, and carbon monoxide poisoning. Although they may be less comfortable for some patients due to confinement, efficacy is not reduced compared to other chamber types.
Multiplace Chambers
Multiplace chambers are equally effective. In fact, studies show no significant difference in outcomes between monoplace and multiplace chambers for most conditions. The advantage of multiplace units lies in the additional monitoring and comfort they provide—staff can be present inside, and the open environment reduces anxiety. This makes them especially suitable for critical care cases or patients who require intensive observation during treatment.
Soft-Shell Chambers
Soft-shell or mild chambers, by contrast, lack proven medical efficacy. Operating at 1.3–1.5 ATA, they do not reach the pressures needed to achieve true hyperbaric oxygen therapy. The UHMS does not recognize them as effective for treating medical conditions other than acute mountain sickness. While some people use soft-shell chambers for wellness, anti-aging, or athletic recovery, clinical evidence supporting these uses is weak, and they should not be considered substitutes for medical-grade HBOT
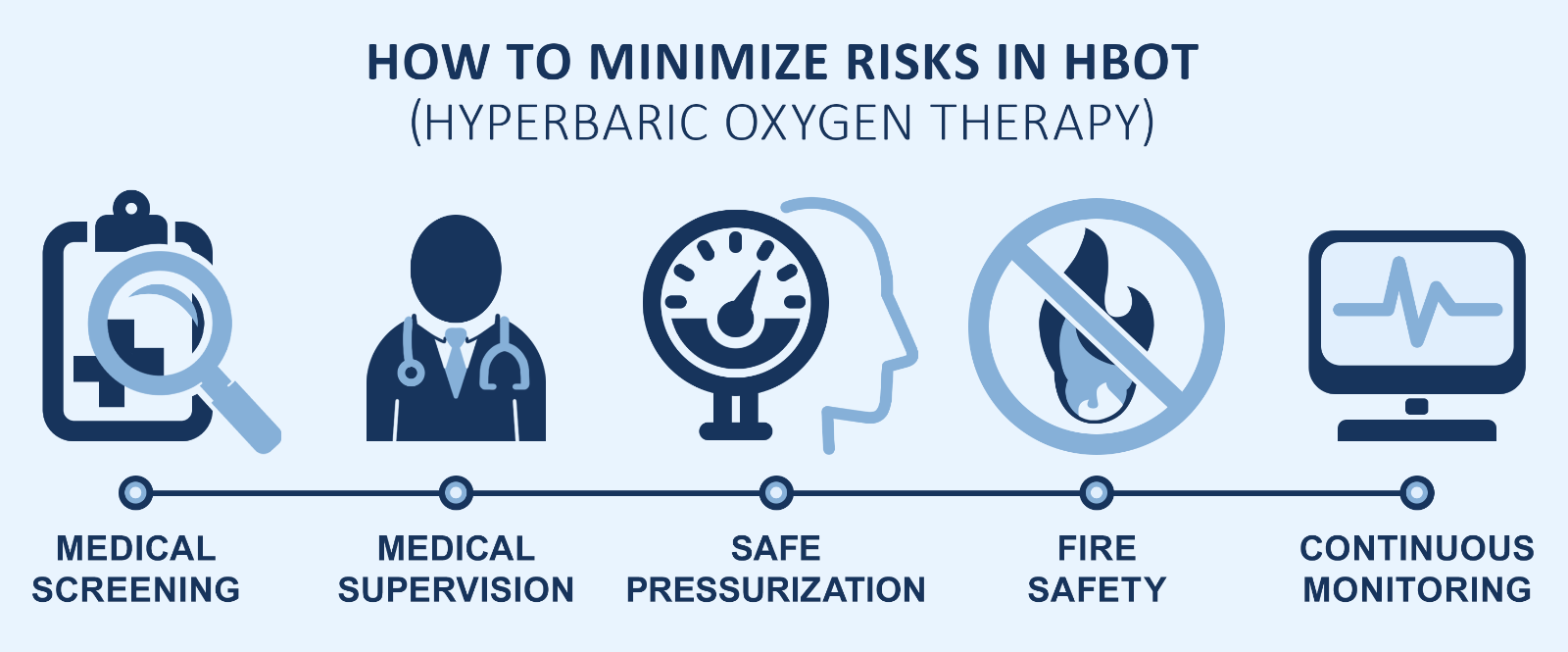
The first step in minimizing risk is conducting a thorough medical screening. Before beginning treatment, patients should be carefully evaluated for their health history, current medications, and any underlying conditions that may be contraindications for HBOT. This ensures that only those who can safely benefit from therapy are admitted into the chamber.
Equally important is having trained medical supervision. Hyperbaric chambers should never be operated without certified hyperbaric technicians, and ideally, a licensed physician trained in hyperbaric medicine should oversee all treatments. Their expertise allows them to quickly recognize and address any complications that may arise.
Safety also depends on how the chamber is pressurized. Gradual compression and decompression are necessary to protect patients from barotrauma, which can affect the ears, sinuses, or lungs if pressure changes are too abrupt. Adhering to proper pressurization protocols is a key aspect of responsible HBOT practice.
Fire safety is another critical concern. Because oxygen greatly increases flammability, strict precautions must be in place. This includes prohibiting lighters, electronic devices, and any other potential ignition sources inside the chamber. Clinics should also maintain rigorous safety checks to reduce this risk.
Finally, continuous monitoring during treatment is essential. Providers should track vital signs and check in with patients throughout each session to ensure comfort and safety. If any discomfort, ear pain, or unusual symptoms occur, the staff should be ready to intervene immediately.
What Patients Should Ask Their Providers
Before starting HBOT, patients should confirm:
Certification
Do they have specialized training in operating and maintaining hyperbaric chambers?
Medical Oversight
Is there a licensed physician trained in hyperbaric medicine overseeing treatments?
Will there be a medical professional available during every dive?
Chamber Safety Standards
Is the chamber FDA-cleared and maintained according to manufacturer and safety regulations?
How often is the chamber inspected and serviced?
Emergency Protocols
Does the staff conduct regular emergency drills?
Are there clear procedures for handling oxygen toxicity, barotrauma, or fire hazards?
Pressurization & Risks
How is the chamber pressurized—using 100% oxygen or compressed air—and what does that mean for fire safety and oxygen delivery?
What pressure levels (ATA) does the chamber operate at, and do they meet the therapeutic threshold recognized by UHMS?
What are the most common risks (such as barotrauma, oxygen toxicity, or claustrophobia), and how does the clinic minimize them during treatment?
Putting Safety First in Hyperbaric Therapy
Hyperbaric Oxygen Therapy can provide life-changing benefits, but only when delivered safely. Patients should educate themselves about the type of chamber being used, understand potential risks, and ensure their provider is qualified and adheres to strict safety standards. Asking the right questions before beginning treatment empowers patients to protect their health while unlocking the healing potential of HBOT.
